For years, bone mineral density (BMD) assessment via dual X-ray absorptiometer (DXA) has been the basic method for assessing fracture risk and diagnosing osteoporosis (Warzecha et al., 2018). Basically, osteoporosis is diagnosed when the BMD T-score at the proximal femur or spine DXA scan is equal to or less than -2.5; however, it is important to point out that 70% of fractures occur in individuals who do not fulfill this criterion. Therefore, it is safe to say that BMD alone does not always predict fracture risk, and additional methods supporting risk assessment are needed (Pothuaud et al., 2009; Wizenneth et al., 2010). In 2012, the US Food and Drug Administration (FDA) adopted the Trabecular Bone Score (TBS) as another diagnostic method for determining osteoporosis (Warzecha et al., 2018). You may ask what exactly is TBS. The TBS is calculated directly from a DXA scan of the lumbar spine area (L1-L4) (Kanis et al., 2015) and is based on the analysis of the optical density texture of the 2D bone density image. In the DXA image, the 2D bone density image is a projection of the 3D bone structure. It sounds a little complicated, but TBS iNsight Software (Medimaps, Pessac, France), which can be installed on existing DXA scanners performs the necessary calculations to determine TBS. A high TBS indicates dense bone microarchitecture (Hans et al., 2011; Winzenrieth et al., 2013), while a low TBS value has been shown to be associated with risk factors for vertebral fractures (Leslie et al., 2013). To date, a majority of studies evaluating TBS as a measure of bone health have occurred in older adult populations and in individuals with specific medical conditions that affect bone health. There is limited research on the effectiveness of TBS in young female/male athletes or specific sport populations.
The question of whether TBS can be used in athletic populations to predict fracture risk has yet to be fully addressed. There have been a few studies (Heinio et al., 2015; Vlachopoulos et al., 2017; Vlachopoulos et al., 2018; Tenforde et al., 2020) in athletes examining TBS and these studies have produced mixed results. Heinio et al. (2015) examined BMD and TBS in a group of female Finnish athletes from a variety of sports with different levels of impact on the athlete’s bone. The authors reported that TBS analysis of the lumber DXA images provided a quantitative method of detecting differences in trabecular architecture of the lumbar vertebrae that was related to bone loading. In addition, the authors reported that this association was independent of lumbar spine BMD. Tenforde et al. (2020) evaluated TBS and spine BMD as predictors in bone stress injury risk in 321 female collegiate athletes from a variety of sports. The authors reported lower TBS scores and spine BMD within athletes who sustained trabecular-rich bone stress injuries. However, the addition of TBS to spine BMD did not enhance the prediction of athletes evaluated for bone stress injuries in this population of female collegiate athletes. The authors concluded that DXA and spine BMD may be sufficient to evaluate collegiate athletes, who are at risk for impaired bone health. In one of the few studies to evaluate TBS in male athletes, Vlachopoulos et al. (2017) reported that adolescent male soccer athletes had higher bone mineral content (BMC) and TBS than male adolescent swimmers and cyclists. In a follow-up study, Vlachopoulos et al. (2018) reported that a 9-month jumping intervention improved both lumbar BMC as well as TBS in male adolescent cyclists and swimmers, but not in the male adolescent soccer athletes.
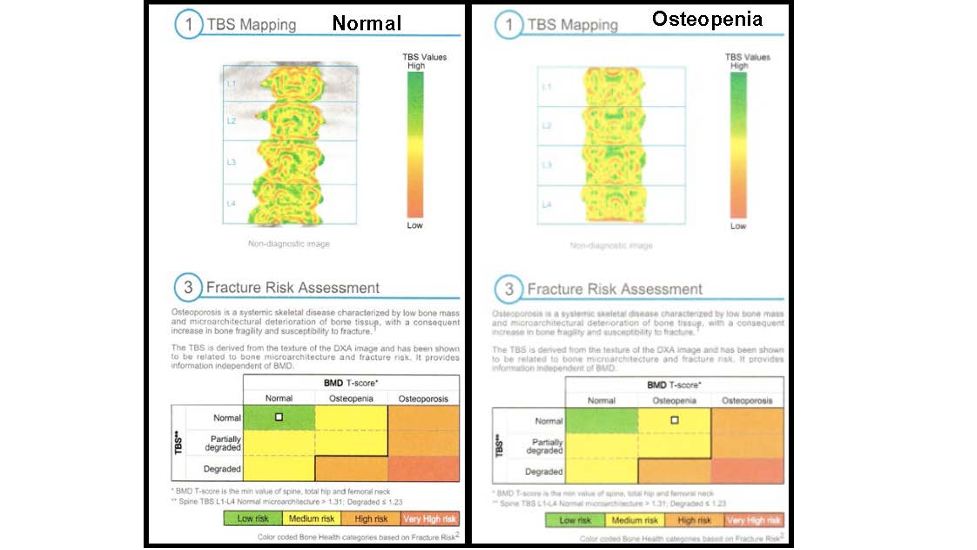
Below is a TBS image from two different individuals. The image on the left is from an individual who has a normal BMD T-score and a normal TBS value. The image on the right is from an individual with a lower BMD T-score. The BMD T-score puts this person at medium risk for osteopenia. Looking at the TBS mapping for the two scans you will notice that higher concentration of green for the image on the left compared to the right image. The larger amount of green represents a high TBS value suggesting great bone microarchitecture. The TBS just gives another way to evaluate this individual and decide whether interventions would be warranted. Whether or not this should be used in deciding whether athletes are at risk for bone stress injuries is still under investigation. However, TBS does provide another way to examine bone health in athletes who may have lower BMD levels.
TAKE-HOME MESSAGE
Although both TBS and spine BMD have been found to be lower in athletes who may be at risk for bone stress injuries it is not clear if TBS enhances the detection of athletes with impaired skeletal health or who may be at an increased fracture risk than just DXA and BMD measures of the lumbar region. Further studies are needed in other athletic populations including male athletes to continue to examine whether TBS can aid in the detection and monitoring of athletes who are at risk for bone stress injuries or fracture.
REFERENCES
Hans D, Barthe N, Boutroy S, et al. Correlations between trabecular bone score, measured using anteroposterior dual-energy X-ray absorptiometry acquisition, and 3-dimensional parameters of bone microarchitecture: An experimental study on human cadaver vertebrae. J Clin Densitom 2011; 14: 302-312.
Kanis JA, Oden A, Harvey NC, et al. A meta-analysis of trabecular bone score in fracture risk prediction and its interaction with FRAX. Osteoporos Int 2015; 26(1): 46.
Leslie WD, Krieg MA, Hans D, Manitoba Bone Density P. Clinical factors associated with trabecular bone score. J Clin Densitom 2013; 16: 374-379.
Pothuaud L. Barthe N, Krieg MA, Mehsen N, Carceller P, Hans D. Evaluation of the Potential Use of Trabecular Bone Score to Complement Bone Mineral Density in the Diagnosis of Osteoporosis: A Preliminary Spine BMD–Matched, Case-Control Study. J Clin Densitom 2009; 12(2): 170-176.
Tenforde AS, Carlson JL, Sainani KL et al. Lower trabecular bone score and spine bone mineral density are associated with bone stress injuries and triad risk factors in collegiate athletes. PM&R 2020; 13: 945-953.
Vlachopoulos D, Barker AR, Ubago-Guisado E, et al. Longitudinal adaptations of bone mass, geometry, and metabolism in adolescent male athletes: the PRO-BONE study. J Bone Miner Resn2017; 32(11): 2269–2277.
Vlachopoulos D, Barker AR, Ubago-Guisado E, et al. A 9-month jumping intervention to improve bone geometry in adolescent male athletes. Med Sci Sports Exerc 2018; 50(12): 2544-2554.
Warzecha M, Czerwiński E, Amarowicz J, Berwecka M. Trabecular Bone Score (TBS) in Clinical Practice - Rewiev. Ortop Traumatol Rehabil. 2018; 20(5): 347-359.
Winzenrieth R, Dufour R, Pothuaud L, Hans D. A Retrospective Case–Control Study Assessing the Role of Trabecular BoneScore in Postmenopausal Caucasian Women with Osteopenia: Analyzing the Odds of Vertebral Fracture. Calcif Tissue Int 2010; 86: 104-109.
Winzenrieth R, Michelet F, Hans D. Three-dimensional (3D) microarchitecture correlations with 2D projection image gray-level variations assessed by trabecular bone score using high-resolution computed tomographic acquisitions: Effects of resolution and noise. J Clin Densitom 2013; 16: 287-296.
About the Author
Donald Dengel, Ph.D., is a Professor in the School of Kinesiology at the University of Minnesota and is a co-founder of Dexalytics. He serves as the Director of the Laboratory of Integrative Human Physiology, which provides clinical vascular, metabolic, exercise and body composition testing for researchers across the University of Minnesota.